Background
Snakebite envenomings (SBE) are an important and neglected health problem due to their frequency and potential for serious clinical outcomes. Envenomations can cause local and systemic complications, depending on the species of snake, the amount of venom injected, comorbidities, timing and use of antivenin, and access to medical care. Systemic effects can be fatal or cause permanent sequelae, including stroke resulting from venom-induced vascular and tissue damage. The aim of this study is to investigate the main clinical and epidemiological characteristics of people who developed stroke after EBD and to identify predictive factors for death.
Methodology/main findings
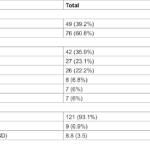
We performed a systematic review and meta-analysis of individual patient data using a predefined search strategy in the MEDLINE/PubMed, LILACS, and SciELO databases, following PRISMA guidelines. A total of 100 studies, predominantly case reports and case series, involving 130 people with stroke after EBM were included. The majority of patients were male (62.3%) and aged between 40 and 59 years (37.7%). Viperids caused 96.4% of snake bites, particularly Daboia russelii and bothrops species Most patients (90%) received antivenom therapy. Reported cases of snakebite-related stroke originated from 22 countries, primarily India (36.9%), Brazil (13.9%), and Sri Lanka (10.8%). Ischemic strokes were more common than hemorrhagic strokes (61.5% vs. 38.5%), and multifocal brain involvement was predominant in both stroke types. The overall fatality rate was 23.4%. Septicemia [OR=6.21 (1.35-33.47); P = 0.001] and thrombocytopenia [OR=3.97 (1.66-10.03); P = 0.02] were predictors of deaths. hemorrhagic stroke [OR=2.67 (1.15-6.31); P = 0.02]multiple brain lesions in a single hemisphere [OR=7.57 (2.33-33.39); P < 0.001]and subarachnoid hemorrhage [OR=7.00 (1.87-29.4)); P = 0.001] significantly increased the risk of death. Motor sequelae remained the most common long-term outcome (22.4%), occurring significantly more frequently in ischemic stroke survivors (28.8% vs 9.4%, P = 0.05). The autopsy findings revealed intense brain alterations generally paralleled by damage to other organs such as the kidneys, lungs and heart.
Conclusions/meaning
EB strokes represent a potential medical emergency in low- and middle-income countries where snakebites predominate and cause high rates of mortality and long-term disability. Recognizing stroke as a disabling and underreported consequence of snakebite is essential to improve clinical outcomes and guide public health responses. Integrating knowledge about predictors of EBD-related stroke death into health policies will be vital to reducing long-term morbidity and promoting disability-inclusive strategies.
Article source: Stroke after snakebite envenomations: a systematic review and meta-analysis of individual patient data Almeida T, Priante SP, João GP, Nery Oliveira D, Mouta G, et al. (2025) Stroke after snakebite envenomations: a systematic review and meta-analysis of individual patient data. PLOS Neglected Tropical Diseases 19(12): e0013789. https://doi.org/10.1371/journal.pntd.0013789
#systematic #review #metaanalysis #individual #patient #data