A solid head in the head does not require that you be a professional football player. More than 3 million people worldwide suffer from a brain shock, also known as mild traumatic brain injury, every year. Some are the result of car accidents, while others are the result of falls or in the heading field in the sports field. After a brain commotion, multimodal rehabilitation and physiotherapy strategies for long -term brain opening recovery are backed by the current clinical practice protocol, which has included cervical dysfunction and vestibular ocular care and effort activity without a sequence of intervention Specific.
Now in a recent study, Columbia University, New York scientists, led by Professor Christopher Wong; Dr. Samantha Vargas, Dr. Tessia Demattos, together with Dr. Lauren Ziaks and Dr. Chelsea Brown of the Park City Hospital, Utah, sought to describe the clinical and informed results of the patient for patients with symptoms after the conversion later of a rehabilitation strategy that addressed cervical dysfunction and benign paroxysmal positional vertigo during the first three weeks of injury, followed by integrated vision and vestibular treatment. The team used existing data 4-5 years ago in a brain shock clinic, and patients examined within the first three weeks after the injury to the treatment for cervical dysfunction integrated with visual and vestibular therapy, which It is consistent with an extended and published brain recovery in the International Magazine of Sports Physiotherapy.
This retrospective cohort study has concluded that patients who received physiotherapy, including manual therapy and exercise for cervical dysfunction and benign paroxys Normality for more than half of the patients. In addition, the deterioration of the vestibular system represented by a clinical measure of the equilibrium capacity, the symptoms of vestibulo-oculomotores and the subjective function of vision of results informed by the patient improved significantly for them, while those taken did not change. However, Benign paroxysmal positional vertigo resolved for all diagnosed before therapy.
In this critical study, Professor Wong and his colleagues showed that a rehabilitation protocol of the conversion -subsequent syndrome, which includes the treatment of cervical dysfunction and the Benign paroxysmal positional vertigo during the first three weeks of injuries, followed by a therapy Visual and vestibular Integrated Clinical improvement and patient- reported results.
Professor Wong said: “The interconnection of the systems makes the care of the sequence to address the musculoskeletal function before the recovery window after the 3 weeks conversion into a clinical approach that then integrates the vision and function of the function of the vestibular system A promising approach to the recovery of brain shock “. This study will help develop a better preferred treatment sequence in clinical practice guidelines for patients with subsequent conversion syndrome.
Diary reference
Wong, CK, Ziaks, L., Vargas, S., Demattos, T. and Brown, C. (2021). Sequencing and integration of cervical manual therapy and vestibulo-oculomotora therapy for symptoms of brain shock: retrospective analysis. International Sports Physiotherapy Magazine, 16(1), 12. 10.26603/001C.18825

Christopher Kevin Wong, PT, PHD
Teacher
Dr. Wong is the curriculum director of the Clinical Residence in Orthopedic Physiotherapy, associate director of the Program in Physiotherapy and rehabilitation professor and regenerative medicine at the Irving Medical Center of the University of Columbia. He teaches and investigates orthopedic issues, orthosis and prostheses, and continues in clinical practice as a certified orthopedic clinical specialist since 2000. His research has been presented in physiotherapy, physiatry and national and international prostheses Conferences and prosthesis conferences and published in more than 50 articles and textbooks.

Lauren J. Ziaks, DPT
Lauren Ziaks has a doctorate in physiotherapy from Northeastern University and specializes in integrating rehabilitation of brain shock for intermountain medical care. Its specialties include vision therapy, vestibular rehabilitation therapy and dysautonomy management.

Chelsea Brown, PT, DPT
Chelsea Brown has a doctorate in physiotherapy from Northeastern University and has developed a clinical interest in the subsequent management of brain shock. She works at an outpatient clinic in the Boston metropolitan area specialized in vision therapy and vestibular treatments.
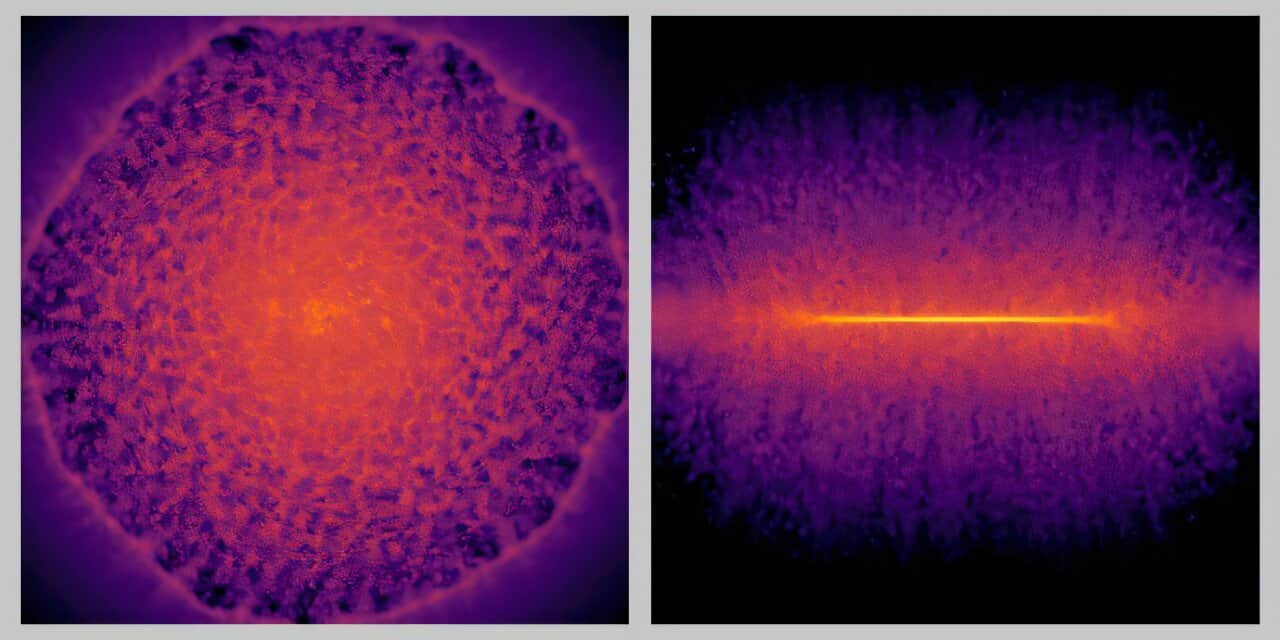
Main image credit: Milius007 of Pixabay
#rehabilitation #strategy #improves #clinical #result #brain #shock #weeks